....leaving the health service in crisis
London (UK) 27 May 2005 - The slow road north from Accra passes roadside businesses with names such as the Life is Not Easy Kiosk and the Fear of the Lord's Kitchen. It is a six-hour journey to Kumasi, Ghana's second city, 200 miles away, and before setting out the coach driver joins the passengers in a prayer.
At the main Komfo-Anokye hospital in the city, you can see why it is important to arrive safely. Hundreds of patients besiege the accident and emergency unit each morning, staffed by a single doctor and a handful of nurses, and serving a city of more than one million.
A critical shortage of medical staff who have been lured away to work in hospitals in Britain and the US is crippling Ghana's health service. The rich countries of the West are systematically stripping the developing world of their doctors and nurses in one of the worst acts of global exploitation in modern times.
The hospital is in a critical state - down to 700 nurses and 320 doctors for its 1,000 beds, half the numbers needed. Its training school turns out almost 100 nurses a year - to be sucked up by the West, lured by the ten-fold salaries. Almost 1,000 nurses and 150 doctors have left Ghana for the UK in the past six years, and the flow is accelerating. Hundreds more have gone to the US, Australia and other countries in a mass migration fuelled by the worldwide demand for medical staff.
At 3pm on a Thursday, there were still more than 100 people waiting to be seen in the accident and emergency unit crammed on to the blue benches under a high roof. A young man stripped to the waist lay full length on the concrete floor, unattended, victim of a mob beating after he had been caught pickpocketing.
As I stopped to talk to Ajala, the mother of Fawuzani, a bright-eyed six-month-old boy with a fractured skull, the injury clearly visible in his misshapen scalp, others crowded round thrusting X-rays at me, begging me to examine their children. A young mother in a red T-shirt pushed her son forward who had large swellings on his head which she described as boils. Another woman with pleading eyes stood her four-year-old in front of me and lifted his T-shirt to reveal a grotesquely swollen scrotum.
Joyce, the chief nurse, brushed them aside with the manner of one long used to dealing with impossible odds. "What can we do? We have one doctor on duty. If we have a road accident - a few weeks ago we had 40 casualties brought here - we must deal with it. The others must wait."
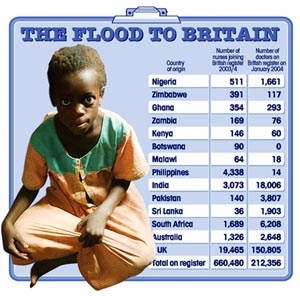
The Lancet today highlights the damaging effect of the exodus of health workers on sub-Saharan Africa, noting that half of the 16,000 extra staff recruited by the NHS in recent years have come from outside the UK and Europe.
More than 30 per cent of practising doctors and nurses in the UK were trained outside the country, compared with 5 per cent in France and Germany, and the demand for health workers from overseas is increasing.
"To poach and rely on highly skilled foreign workers from poor countries in the public sector is akin to the crime of theft," The Lancet says. The effects can be seen in Ward A1 on the maternity unit of Komfo-Anyoke hospital. The crush is overwhelming - mothers and babies crammed into every corner - on the beds, between them and under them. A blackboard in the office of Margaret Boafo-Atiemo, the director of nursing, reveals that on the previous day, 18 May, there were 207 maternity cases of whom 52 were accommodated on the floor. One mother and three babies died - as many as would perish in a year at a similar sized British hospital.
A fourth baby died in front of me a few minutes later. Up on the special care baby unit, where 65 babies are looked after by four nurses in three wards, incubators line the walls and iron cots are ranged side by side down the centre. It is impossible for four nurses to monitor the condition of so many severely ill babies whose condition can become critical in minutes. As we walked round the high dependency unit I noticed a baby with thick mucus dribbling from its mouth. It had stopped breathing and the nurses began urgently massaging its tiny chest and sucking the secretions from its nostrils. It responded but it was too late. "It is in a bad state. There is no hope," said Regina Obeng, the nurse in charge of the unit. The baby's chest shuddered but its breathing was irregular and it soon failed again.
"The number of bad cases is rising," she added. "They come with conditions that might have been prevented if the babies had been resuscitated sooner after birth. But because the midwives come late they are much harder to resuscitate. If we had enough doctors and nurses in the community it would prevent babies coming in a bad state."
A day later in Accra, I sat with Anastina Bakokor under the whirring fans in the sweltering out-patients department of Ghana's main hospital as she was told that her son, Lord, born four weeks ago, is brain damaged - the result of a difficult, unrecognised breech delivery and a long delay in resuscitation.
He is one of scores of babies admitted to the neonatal intensive care unit of Korle Bu teaching hospital with asphyxia because they have not been properly monitored during birth.
Now that lapse, in a chronically over-stretched health service, has changed his life - and hers - forever.
Korle Bu hospital, on the western edge of Ghana's traffic-choked capital, has barely half the medical staff it needs. Its 16 operating theatres function only in the mornings. One of the two theatres serving the maternity department is closed because of a shortage of anaesthetists and nurses. When a crisis occurs during labour, mothers cannot rely on an immediate Caesarean but must wait their turn - at the risk of catastrophic harm to their babies.
As she struggled to absorb the implications of what she had been told, Anastina busied herself booking appointments for her damaged son. Nurses pushed piles of dog-eared folders about their desks as 50 other new mothers, all clad in celebratory white, waited their turn.
Later, sitting on a bench in the gloomy children's block, with its faded rainbow, she started to weep. "At first they said he may be affected but now it is definite. His limbs are too rigid. It is very painful. I don't mind if he is not good at school but if he can't walk or talk - if he can't read - what will he do?"
Anastina is neither downtrodden nor poor, her husband works as a technician for Ghana Telecom, but she is powerless against the global forces that have sealed her family's fate. She permitted a photograph of her son but declined to be pictured with him. "Someone might recognise me," she said.
Alongside her, Joyce Wilson, 33, carries her lanky, sleeping four-year-old son, Frank, brain damaged at birth - a victim of the lack of staff to monitor new borns at home. As she manoeuvres him on to her back to carry him home, his long limbs flop uselessly. "Life must go on," she says with a smile.
At the weekly meeting of the hospital's directors, Professor Frimpong-Boateng spelt out the impact of the lack of staff.
"We have a handful of midwives in the country and they are not able to monitor women in labour. At least 60 per cent of the babies in the neonatal intensive care unit were born at full term but were deprived of oxygen at birth because of the lack of staff - something that would be rare in the UK."
In this poverty-stricken country, where many families survive on ?30 a month, the high medical bills that follow a spell in intensive care have a shocking consequence for the mothers who have spent agonising weeks worrying whether their children would live or die. Babies discharged from the intensive care unit - a beacon of excellence amid the dilapidated buildings - are transferred to a side room to await payment of the bill.
But many parents cannot afford the cost. I counted 27, carefully swaddled babies lying on four black mattresses on the floor - held hostage because their parents could not pay.
Their mothers are allowed into the unit every three hours to feed their offspring but are prevented from taking them home until they have raised the cash. It is a prison for babies.
Some had been detained for more than a month awaiting payment of bills ranging from 1.5 million to 11 million cedis (?90 to ?650) - more than a year's salary for an average worker.
They are bills that might have been avoided if there had been sufficient staff to provide proper care for their mothers. The Ghanaian government subsidises health care but each hospital sets its own fees. "All the time I was praying," said Zuleiya Huseini, 24, whose son was born unable to breathe and had just been discharged after three weeks of treatment. "Now I don't know what to do."
She was left for two hours in the second stage of labour, which would have led to a clinical negligence claim in Britain. It is the stage when the cervix is fully dilated and the mother starts to push, which should last no more than 10 to 20 minutes, or there is a risk to the baby of oxygen deprivation and brain damage. Now she faces a bill of 5,686,600 cedis (?330) for the time her son spent in intensive care, and she will not know for weeks or months whether he has been permanently affected.
Her husband sells fridges but the business has "gone bad", she says. As the doctor explains how much she owes, tears well in her eyes and spill down her cheeks.
The doctor's tone does not change. Compassion is not the African way - suffering is too widespread and the professionals too thinly stretched. "The government cannot take care of the bills of all the children," he says. "But if you are earning a dollar a day and face a $500 bill it is heavy."
The consequences of the chronic staff shortages can be seen everywhere - in grossly overcrowded clinics and wards which mean long waits, poorer care and problems missed. Infant mortality is on the rise - up from 55 per 1,000 live births in 2003 to 64 last year.
In the children's emergency room, a holding area for those too sick to be sent home when there is no space on the wards, a two-year-old girl who has accidentally drunk kerosene is stretched out on a bed. She vomited and then inhaled, damaging her lungs. She lies with her arms raised to ease her breathing, looking fearful, next to a girl sick with Aids.
Wendy Ogbarmey-Tettey, the nurse in charge, said: "This is calm. Some days we have 80-90 patients in the 20 beds. The patients do not get the quality of care they should have."
There are some grounds for hope. At Komfo-Anokye hospital a new maternity block is half built and a children's block has been started that will ease the congestion when they are complete, the first expansion of the departments since the hospital was built in 1955.
But bricks and mortar are easy to come by compared with medical expertise. When I asked Kwame Frimpong, spokesman for the hospital, how the new unit would be staffed, he said: "That is the problem. If we don't get the staffing right it will be a white elephant."
Yaw Manu, consultant, Milton Keynes hospital
Dr Yaw Manu, 60, came from Ghana in 1997 as a medical officer. He works in Milton Keynes General Hospital as a consultant radiologist.
"I came to Britain to do a postgraduate course, because in those days we did not have a postgraduate facility in Ghana. If you wanted to do further academic study, you had to go abroad. I contemplated going to the United States, but came to Britain because I had some relations living here and I was accepted at Liverpool University.
"I thought I was going to be here for three years and I had every incentive to go back. I had a good lifestyle there and a senior figure at the hospital I was working at said when I came back I could become a department head. But just as I gave in my notice to Liverpool health authority in 1981, I found out there had been a coup in Ghana and it was particularly violent.
I phoned my mother in Ghana and, knowing I was a political person, she advised me not to go back until we knew how the future was going to pan out.
After working in Watford, I got another job in Liverpool and got settled. I had two sons and I wanted to put them both through boarding school in Britain.
"Since 1992, I have gone to Ghana at least every year and I have a house in the capital. When I retire, I will divide my time between here and there, but I have grandchildren in Britain so I can't cut my ties. Every time I go to Ghana, I go to a teaching hospital and give as much advice as I can."
Eben Badoe, consultant, Korle Bu hospital
Eben Badoe, a consultant paediatrician at Korle Bu hospital in Accra, spent 10 years working in London and Bristol before returning in 2000. "It is not just about money. You don't need that much to make you happy. It is what you contribute," he said.
"Everything has been done medically in the West. But here you can contribute. In terms of the clinical work, what we see here is unsurpassed. This hospital is a living museum.
"In the UK you are nothing, here you are a champion. I have never met Tony Blair but here I am invited to parties with the President. It does not put money in my pocket, but it makes me feel good."
A top hospital consultant earns around ?7,500 a year in Ghana and a senior nurse about ?2,000. In the UK their salaries would be 10 times higher. [emphasis added]
The entire class of doctors that graduated in 2002 has either left or is planning to leave, according to the Medact report. Overall, more than 50 per cent of doctors who have qualified in Ghana have already left the country.
Kofi Agyeman, 30, who qualified in 2000 and is specialising in paediatrics at Korle Bu hospital, works six days a week for up to 60 hours. He earns around ?200 a month.
"A lot of my classmates are already away in England and America. We are always in contact, we talk a lot," he said. He will not reveal his plans but he is frank about the temptations - better pay and an easier life.
UK versus Ghana
Child mortality: deaths before 5
Ghana: One in 10
UK: One in 150Life expectancy at birth
Ghana: 57.6 years
UK: 78.2 yearsSpending on health per head
Ghana: ?7
UK: ?900Births with a midwife present
Ghana: 44 per cent
UK: 100 per centDoctors per 100,000 people
Ghana: 9
UK: 166Nurses/midwives per 100,000 Ghana: 84
UK: 540