Eight Los Angeles-Area Residents Charged ... in Nationwide Medicare Fraud Strike Force Takedown Total of 107 Defendants Charged in Seven Cities for Approximately $452 Million in False Billing
LOS ANGELES—Eight Los Angeles-area residents, including two doctors, were charged today for their roles in schemes to submit more than $14 million in false billing to Medicare, announced the Departments of Justice and Health and Human Services (HHS).
The charges in Los Angeles are part of a nationwide takedown by Medicare Fraud Strike Force operations in seven cities that led to charges against 107 individuals for their alleged participation in schemes to collectively submit more than $452 million in fraudulent claims to Medicare. This takedown involved the highest amount of false Medicare billing in a single takedown in strike force history.
“The results we are announcing today are at the heart of an Administration-wide commitment to protecting American taxpayers from health care fraud, which can drive up costs and threaten the strength and integrity of our health care system,” said United States Attorney General Eric Holder. “We are determined to bring to justice those who violate our laws and defraud the Medicare program for personal gain. As today’s takedown reflects, our ongoing fight against health care fraud has never been more coordinated and effective.”
“Medicare fraud drains vital resources and harms consumers across the nation,” said United States Attorney André Birotte Jr. “The problem is national in scope and it calls out for the type of coordinated national response that today’s crackdown represents. This office is dedicated to working with all our partners, both locally and nationally, to protect this important public program that serves our elderly and disabled.”
“As today’s strike force operation demonstrates, health care fraud is not limited to just one or two types of health care providers,” said Glenn R. Ferry, Special Agent in Charge for the Los Angeles Region of HHS’s Office of Inspector General (OIG). “Whether it is a physician, a business owner, or any other provider, OIG and our law enforcement partners are committed to pursuing those that attempt to steal precious dollars from the Medicare program.”
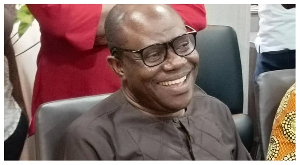
According to court documents filed in the Central District of California, two Orange County doctors and two of their co-schemers were charged for allegedly submitting nearly $5.7 million in false claims to Medicare for durable medical equipment (DME). Specifically, the defendants billed Medicare for enteral nutrition, a liquid nutritional supplement. Medicare will only pay for enteral nutrition if a patient has a feeding tube. According to the indictment, Dr. Augustus Ohemeng, 62, of Buena Park, and Dr. George Tarryk, 72, of Seal Beach, wrote fraudulent prescriptions for enteral nutrition for patients who did not have feeding tubes. Co-defendant George Samuel Laing, 41, of Sylmar, who managed the clinic where Tarryk and Ohemeng practiced, allegedly received kickbacks in exchange for referring the prescriptions to Ivy Medical Supply, owned by co-defendant Emmanuel Chidueme, 59, of Mira Loma. Ivy then fraudulently billed Medicare for the enteral nutrition, even though it was not medically necessary and was not delivered to patients in the quantities billed to Medicare. Ohemeng, Tarryk, Laing, and Chidueme were arrested this morning and are scheduled to make their initial appearances before a U.S. Magistrate Judge this afternoon.
“The charges announced today emphasize disturbing health care fraud trends, including the arrest of physicians, that exploit federal health care meant for those in need,” said Steven Martinez, Assistant Director in Charge of the FBI’s Los Angeles Field Office. “The cases charged in Southern California and around the U.S. indicate the staggering amount of fraud adversely affecting the U.S. economy and illustrate the need for the continued focus on protecting federally funded health care programs.”
In a separate case, two defendants were arrested on charges related to their DME company, Latay Medical Services, which allegedly submitted more than $8 million in fraudulent billings to Medicare for power wheelchairs, orthotics, and hospital beds that were either not provided or were medically unnecessary. The indictment charges Latay’s owner, Bolademi Adetola, 46, of Harbor City, and Latay employee Yuri Martin Lopez, 46, of Lawndale, with obtaining fraudulent prescriptions for the DME, creating fake documentation to make it seem as though the DME had been delivered when it had not, and delivering DME less expensive than that listed on Latay’s Medicare claims.
Two additional defendants are scheduled to self-surrender today on charges related to Greatcare Home Health Inc., a home health agency that received more than $5.4 million from Medicare for skilled nursing and physical therapy services that were often either never performed or performed by unlicensed individuals. Greatcare’s owner, Hee Jung Mun, also paid illegal kickbacks to doctors, individuals known as marketers, and patients themselves in order to recruit Medicare beneficiaries. Mun, along with three other Greatcare employees, have already pleaded guilty to the fraud and are awaiting sentencing before U.S. District Judge Dean D. Pregerson. Yeong Ja Lee, 50, of Mid-City, is scheduled to make her initial court appearance this afternoon on charges that she visited and provided services to patients without a license and created false documentation for Greatcare and one of its referring doctors. Sang Whan Ahn, 60, of Koreatown, is also scheduled to appear on charges that she acted as a marketer, accepting kickbacks in exchange for referring patients to Greatcare.
As a part of the operation, members of the strike force in Los Angeles also executed three search warrants today.
The Medicare Fraud Strike Force operations are part of the Health Care Fraud Prevention & Enforcement Action Team (HEAT), a joint initiative announced in May 2009 between the Department of Justice and HHS to focus their efforts to prevent and deter fraud and enforce current anti-fraud laws around the country.
Since their inception in March 2007, strike force operations in nine locations have charged more than 1,330 defendants who collectively have falsely billed the Medicare program for more than $4 billion. In addition, the HHS Centers for Medicare and Medicaid Services, working in conjunction with the HHS-OIG, are taking steps to increase accountability and decrease the presence of fraudulent providers.
The cases announced today are being prosecuted and investigated by Medicare Fraud Strike Force teams comprised of attorneys from the Fraud Section of the Justice Department’s Criminal Division and from the U.S. Attorney’s Offices for the Central District of California, the Southern District of Florida, the Eastern District of Michigan, the Southern District of Texas, the Middle District of Louisiana, the Northern District of Illinois, and the Middle District of Florida; and agents from the Federal Bureau of Investigation, HHS-OIG, and state and local Medicaid Fraud Control Units, including the California Department of Justice and Los Angeles Sheriff’s Department’s Health Authority Law Enforcement Task Force.
An indictment is merely a charge and defendants are presumed innocent until proven guilty.
Diaspora News of Tuesday, 8 May 2012
Source: http://www.fbi.gov
Ghanaian Doctor Charged in Nationwide Medicare Fraud