Ghana has over the years rolled out a number of interventions with the aim of reducing the incidence of malaria, yet the level of morbidity is still high in the country.
Malaria still accounts for 40 percent of all outpatient attendance, with the most vulnerable groups being pregnant women and children under five (5) years.
The incidence of malaria, according to the Ghana Health Service (GHS) increased by 3.5 percent in the first quarter of 2016. This was mainly attributed to poor drug treatment practices.
Between January and March 2020 alone, the country has recorded a total of 1,001,070 malaria cases with 54 deaths. Of the figures, 21,201 are children under five years.
Malaria control protocols
In 2014, the Ministry of Health (MoH) in accordance with international guidelines for case management of malaria, indicated that all suspected cases of malaria must be tested by Rapid Diagnose Test (RDT) or microscopy before treatment.
But interestingly, home based remedies that involve over the counter and left-over drugs as well as use of uncertified herbs are often the first treatment strategies for malaria treatment for most Ghanaians.
More often than not, individuals only visit a health facility after such remedies have proven ineffective and their conditions have gotten worse.
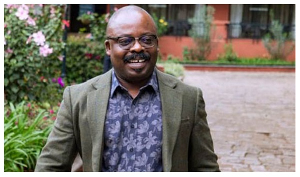
Dr Emmanuel Ofori, a Senior Medical Officer at the Cape Coast Teaching Hospital (CCTH) says, compliance of “test before you treat” among patients are generally low.
According to him, people do not test but still go to the drug store or pharmacy to buy malaria drugs, while others still treat for malaria even if they test negative with various flimsy excuses.
“I have had adamant patients who after testing negative for malaria still think they have malaria and would go ahead to buy malaria drugs to treat,” he revealed adding that “it is real. People are buying at the counter all the time”.
Mr Kwabena Nimako, a Pharmacist at the CCTH agrees with Dr Ofori and says compliance to malaria protocols among the general public is low.
“The government has put in place preventive measures, but compliance have been a big issue. “People are not complying, they are not sleeping in mosquito nets, they are staying out late at night, there is poor sanitation that is why malaria is still one of the top ten OPD cases in the Country,” he indicated.
Mr Nimako said as per the malaria control programme, before any malaria drug is dispensed to a patient, the person must test positive.
But according to Dr Ofori, the pharmacies though are aware of the policy on malaria, sell malaria drugs to people while they have not done the test.
He insisted that “the first thing to do is to test to be sure the person has malaria prior to administering any form of treatment”.
Dr Ofori admitted that even health professionals faced a difficult challenge in diagnosing malaria, “the rapid test is not 100 percent, it is not conclusive. You could test negative and still have the parasite,” he added.
Self-medication and home-based treatment
According to research, about 69 percent of urban poor communities in Ghana self-medicate and resort to herbal medications as the first response to suspected malaria.
Health insurance status, economic status, level of social support, and area of residence are associated with one seeking alternative treatment for malaria relative to orthodox treatment.
Many of the people interviewed for the purpose of this article admitted to having engaged in self-medication for malaria treatment with only a handful saying they always went to the hospital.
“I only go to the hospital when I have severe malaria but if it is not so serious, I just go to the drug store to buy some malaria drug”. This was a response from Madam Sarah Koomson when asked about her first point of call when she experienced symptoms of malaria.
Another person, Mr Joseph Bentsil provided a similar response and explained that it was convenient.
Mr Nimako expressed worry about the practice of home-based medication as treatment for malaria and indicated that such practices may provide negative feedback for the government and largely impact policy decisions.
“It is worrying when people are treating malaria at home. That does not give us the real facts about malaria prevalence because it is only when people come to the hospital for treatment that we will know the exact number of people infected by malaria which will inform any policy decision,” he explained.
He warned that taking malaria drugs without testing could have serious implications for the person.
“Under normal circumstances, if you have the malaria parasite, when you take the medicine, it will fight the parasite. But here is the case that people take the medication when there is no parasite to fight. So it will rather fight on other organs to make the whole situation become complicated,” Mr Nimako explained.
Traditional and Alternative Medicine is allowed but...
Regarding traditional and herbal medication, Mr Nimako said its abuse was what has given it a bad image.
“As we all know, people are mixing concoctions and using them to treat malaria and all sorts of illness,” he said.
That, he said, was the reason why the Ministry of Health (MoH) was streamlining all traditional medicine to incorporate them into the formal health system such that patients could opt for traditional medicine against the orthodox.
The move, he said had resulted in some hospitals in the country setting up traditional medicine units where patients who prefer traditional medication were treated with certified herbal medicines.
“I have had some people who rejected the orthodox medication, saying they are not as effective as herbal medicine,” Mr Nimako said.
Mr Osman Gambo, a resident of Cape Coast, shared his experience with herbal medication and said herbal medicine had always proven effective whenever he was used to treat malaria.
But Mr Nimako advised that “even if you prefer the traditional medicine, you still have to visit the hospital and test for malaria before you use it”.
“Go to the hospital and ask for a certified herbal malaria drug and it would be given to you,” he advised.
Education
Mr Nimako largely attributed the practice of self and home-base medication as well as the use of uncertified herbal concoctions to the fact that education had not gone down well with the people.
Though a lot of education and sensitisation is being done, he admitted that more education was needed to make the public understand the issues, and visit the hospital for malaria treatment.
Way Forward
Dr Ofori wants stakeholders to address the underlying deterring factors that make the formal health sector unattractive to clients to be addressed.
He indicated that such deterring factors, which include bad staff attitude, time wasting and poor customer relations, badly affected the quality of health care provision.
According to Dr Ofori, there was too much time wasted in accessing health care which was very detrimental to the health of patients and the facilities as well and therefore it must be addressed urgently.
“A market woman for instance will not go to the hospital to spend long hours. She will never do that unless she is dying,” he said.
“Herbalists are all around them, they are very close to them. How close is the CHPS compound or health facility to the community and even if they go, do they get the required attention and medication?” he quizzed.
Dr Ofori believes that if the above mentioned issues are holistically addressed to improve standards, reduce time wasting among others, patients would be willing to visit the hospital whenever they experienced symptoms of malaria knowing that they would not spend longer time at the hospital.
Mr Nimako advised Ghanaians to desist from the habit of treating malaria at home to avoid complications leading to serious financial burden or even death.
“I will advise each and every one, though we are not in normal times, but because we do not want to complicate issues, everyone should come to the hospital for malaria treatment”.
Conclusion
Data from the GHS shows that malaria related deaths had reduced by almost 91 percent and its prevalence among vulnerable groups such as children under five years and pregnant women had reduced since 2010.
This is a massive achievement but to sustain the gains in the midst of the COVID-19 pandemic, is overstretching the health system more than it could withstand, because people fear to report and come in when their conditions have worsened.
The World Health Organisation (WHO) have admonished countries to intensify malaria interventions as COVID-19 rages on.
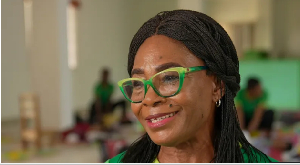
Ms Helen Amegblor, a concerned health worker, encouraged the Government and the GHS to do more, using structures and resources at their disposal to sustain the gains made.
“Now more than ever, it is critical that we safeguard these gains so that we do not see mortality cases on two fronts, (i.e malaria and COVID-19). If we need to integrate malaria with COVID-19 messages for a wider reach, let us begin to do it,” she stated.
This article was produced as part of the People for Health (P4H) project being implemented by SEND Ghana, Penplusbytes and the GNA with the aim of reducing inequities in the delivery of health services through promotion of good governance practices of accountability, transparency equity and participation.
Health News of Monday, 17 August 2020
Source: GNA