Since the beginning of the year there have been sporadic strikes by health workers across Ghana. Pretty much of the reasons rest on pay issues, but at deeper level it reveals schism between Ghanaian traditional medicine and the formal orthodox medicine. This has been a recurring matter in most part of Ghana’s 50-year existence, especially as economic conditions worsen. While public health workers deserve good pay, like other professionals, their problems are increasingly being worsened by mounting health problems and population increases. This calls for sober and holistic reflection of the entire Ghanaian healthcare delivery system.
The burden on public healthcare delivery system in Ghana will be made lighter if traditional medicine, of which 80 per cent of Ghanaians access, is further integrated into the healthcare system as the Indians and Chinese, among other Southeast Asian states, have done. The integration of traditional medicine into the formal healthcare system will also give value to the increasing call by international health experts for more “focus on primary health care” that will “enable people to increase control over the decisions affecting their health through primary health programs that link with community development or empowerment,” as Dr. Gretchen Roedde, of the University of Ottawa’s Medical School, told an international health conference in Ottawa recently.
At the centre of Ghana’s healthcare system is serious shortage of health workers. Ghana’s case feed into the fact that despite unprecedented advances in health care, the world is immensely confronted with severe shortages of health workers, especially in the poor countries such as Ghana. WHO and Lincoln Chen and associates report that sub-Sahara Africa alone needs about 1 million health workers. Meanwhile, at the other end health workers shortages large number of traditional health workers are waiting to be refined and integrated into the formal healthcare system. Wisdom demands that the two are integrated beautifully to give respectability to Ghanaian traditional medicine. One key attempt is to debunk the long-running notion that traditional medicine is backward. Dr. Ibrahim Samba, World Health Organization (WHO)’s Africa Regional Director, explains that even though African traditional medicine has often been stigmatized as a backward practice during colonialism, it has continued to strive because it is culturally accepted and accessible to more than 80 per cent of Africans.
Such attempts to correct the historical wrongs against Ghanaian/African traditional medicine come in the face of growing world-wide use of traditional medicine. The World Bank, WHO and other agencies report that in Europe, North America and other industrialized regions, over 50 per cent of the population have used traditional medicine at least once. In San Francisco, London and South Africa, 75 per cent of people living with HIV/AIDS use TM/CAM. Seventy per cent of Canadians have used complementary medicine at least once. In the United States, 158 million of the adult population use complementary medicines and according to the USA Commission for Alternative and Complementary medicines, US$17 billion was spent on traditional remedies in 2000. The global market for herbal medicines currently stands at over US$60 billion annually and is growing steadily.
WHO and its associates explain that in the African region, traditional medicine is better integrated in Ghana’s health care system compared with other African countries, where there are mutual distrust between traditional healers and conventional medicine. One of the seven directorates of Ghana’s Ministry of Health is Traditional and Alternative Medicine (TAM). It is charged with the planning and development of TAM policy. It is estimated that 70 percent of Ghanaians depend solely on the health care provided by approximately 45,000 traditional healers, most of who are recognized and licensed through various associations that fall under the nationally mandated Ghana Federation of Traditional Medicine Practitioners’ Association. Ghana also has passed several decrees to regulate and ensure the safety of traditional medical practices such as homeopathy, naturopathy, and osteopathy among others.
One of the key vehicles to integrate traditional medicine into Ghana’s health care system is the mechanism of decentralization. In line with changing attitudes towards democratic governance, international inclinations favour decentralization in support of primary health care, of which traditional medicine should be its key driver. In Ghana, as in other African states, decentralization of the health care system is in response to poor economic conditions, poor logistics, and reduced public finance for health services. In the U.N Human Development Index, which measures the well-being of nations world-wide, Ghana is ranked 136th out of 177 countries ranked in 2006. This means Ghana is not doing well as it’s demographic, socioeconomic and health statistics reveal, worsened by frequent strikes by its 51, 910 health workers.
Though PNDC Law 207 (1988) provided the framework for decentralization of Ghana’s healthcare system, it failed to formally integrate traditional medicine into the system, especially at the local levels. Though the law transferred wide ranging functions, powers and responsibilities to District Assemblies, including legislation, budgeting revenue collection, political and social development, etc, it did not include traditional institutions in the broader sense of Ghana’s development process. Though it aimed to enhance efficiency and responsiveness to local health needs by shifting some of the burden of financing health care from the public sector to the beneficiaries and also shifted some decision-making from central planning agencies to those in closer touch with local conditions and user needs, traditional medicine was left out as an integrated scheme.
In heavily rural-based population, traditional healers/workers are the only source of health services for majority of Ghanaians/Africans and in most cases; they are the preferred source of health care. In Ghana, every 1 traditional healer attends to 200 patients, while 1 doctor attends to 20, 000 patients, according to Erick Gbodossou and associates. The traditional healer has more time to attend to his/her patients than the orthodox doctor. It is estimated that over 85 per cent of sub-Saharan Africans access their health education and health care from traditional healers. Traditional practitioners far outnumber modern health care practitioners, are culturally accepted and respected, and more universally located.
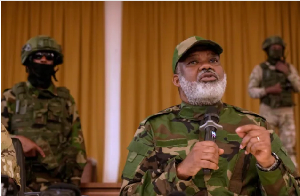
Indications from demographic, socioeconomic and health statistics demonstrate that Ghana’s health care delivery problems could be alleviated by integrating traditional medicine, healers and workers into the health care delivery system. Health Minister, Courage Quashigah and his bureaucrats may be attuned to this but more is needed in this direction.