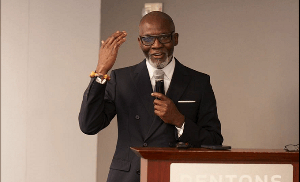
A Public Health Practitioner based in the United Kingdom, Dr Da Costa Aboagye has observed that there is a huge gap between the National Health Insurance policy and real life which according to him leaves much to be desired.
According to Dr Aboagye opines that much needs to be done in Ghana to address social determinants of the National Health Insurance Scheme in a bid of improving the health sector.
World conference of Public health promotion
Speaking at the 22nd World conference of Public health promotion on “The National Health Insurance Scheme in Ghana: Policy and Equity” in Curitiba Brazil, Dr Da Costa Aboagye said, the much talked about “universal health coverage” as a sustainable development goal can only be meaningful, if Ghana improves the quality of health services, ensures that they are more safe, equitable, effective and patient-centred.
According to him, Ghana like many African countries was not able to meet the Millennium Development Goals by the 2015 deadline despite the massive resources deployed.
While this performance can be attributed to several factors, Dr Aboagye attributed the main causes to be the absence of systematic and coordinated action on social determinants of health, which he said is outside of the health system and NHIS.
Towards improving accessibility
In a suggestion to address the issue, the health policy and impact assessments expert argued that Ghana can work towards improving the accessibility of its health services – in terms of transportation, education, employment, geography, gender, age and financing especially for the worse-off in society but in addition, continuously prioritizing the quality of these services.
He said improving the health of Ghanaians will entail coordinated action across the health and non-health sectors to bridge the National Health Insurance and health policy implementation gaps, increase access and reduce inequities that are not only unnecessary and avoidable but unfair.
Touching on his research work in Ghana in the presentation, the Leeds fellow explained that the National Health Insurance Scheme technically covers the core poor, in practice, but due to the very exclusive definition of the core poor and challenges of identifying those who qualify, very few poor people are actually covered.
Poverty
Backing his findings, the UK based public health promotion and health insurance financing connoisseur emphasised that “the well-defined factors of poverty seen in Ghanaian communities are not the same as the official determinants used as criteria for exemptions under the nationwide National Health Insurance Act (LI) 1809” as no source of income, no identifiable residence and not receiving support from others.
Demonstrating his findings, he noted that the poor are struggling to manage the National Health Insurance Scheme by sacrificing basic needs such as food and clothing or having to borrow to pay for health services out of pocket, an aim the pro-poor National Health Insurance Scheme has failed to achieve more than ten years after its inception.
“Poor people and their families are making extraordinary food sacrifices to obtain and pay for National Health Insurance. There is therefore a gap between National Health Insurance Scheme policy and real life” – the Director of Health Impact Assessments (HIA) and Policy Consult Limited in the United Kingdom postulated.
He further praised the Gender and Social Protection Ministry in Ghana for their active role in the National health insurance registrations for some of the most vulnerable population in society but emphasised that there is much work to be done to “closing the gap.”
Dr Aboagye urged government, policy makers and stakeholders to strengthen health promotion practice based on social determinants of health to address these lapses in the light of the sustainable development goals.
“This means the National health insurance scheme and the Ghana health systems must build an integrated system far from the current biomedical concept emphasis,” he added.
This, Dr Aboagye noted will be in line with the World Health Organisation’s Commission on Social Determinants of Health’s report in 2008, the United Nation Platform on Social Determinants of Health in 2013 and the United Nations Panel on Sustainable Development Goals on Health in 2015 – to improve the quality of health services in Ghana such that they are more safe, equitable, effective and patient-centred so that “universal health coverage” is a meaningful sustainable development goal.
The conference which was under the theme “Promoting health and equity” was attended by high level officials from WHO, NGO’s , experts from Health systems and Global Health, Public health policy consultants, Lecturers, Researchers, Students, Government and elite stakeholder representatives from various continents including North and South America, Asia, Africa and Europe.
Health News of Wednesday, 25 May 2016
Source: Da Costa