After eight years of fighting…
We never stopped saying the very things some hated to hear about reforming mental healthcare in Ghana Dr Akwasi Osei, Chief Psychiatrist
Eight years ago, there was no mental health law, no definite plan for integrating mental health care into mainstream service and no plan for addressing its forbidding human resource challenges.
As of May 2012, with the passage of the Mental Health Law, Dr Akwasi Osei, Chief Psychiatrist, is full of optimism for the prospects of mental healthcare in Ghana.
“The future is very bright. No doubt about it”
Even so, the mental health front, under Dr Akwasi Osei’s inspiring and unyielding leadership, recognizes the need not to rest on their oars. The new law provides a six month period during which certain structures are to be operationalized to give it full steam. By October 2012 therefore, it is expected that a Mental Health Board would be established with the key function of overseeing the drafting of a legislative instrument to operationalize the new law. Not wanting to be overtaken by events, a technical coordinating group has already been constituted to present a draft legislative instrument for the consideration of the Board the minute it is finally established.
The law specifically makes provision for a mental health fund with fund managers appointed by the Board. Sources of funding are to be defined by Parliament. Possibilities include allocating a component of existing levies (VAT) or establishing a new levy. Others are to integrate funding for mental health activities into regular cycle of annual government budgeting. Finally, the Board may also source research grants etc.
What is unique about Ghana’s mental health law?
Firstly, it promotes a community oriented approach, a clear departure from the existing facility based care. Secondly, it incorporates the informal sector of unorthodox mental health practitioners in acknowledgment of the 70% of the population already being catered for by them. Dr Akwasi Osei explained this incorporation to mean identification of the numerous prayer camps that attend to the mentally ill, provision of training support and regulation of their practice including the application of sanctions should they overstep approved boundaries. These unorthodox practitioners have thrived mainly due to sociocultural beliefs and partly as a reflection of the weak capacity of the formal health sector to provide adequate care for the mentally ill.
“They can no longer put the mentally ill patient in chains or shackles. If the patient is violent, you may restrain but ensure referral to the hospitals within 48 hours” spells out Dr Akwasi Osei. In addition to offering prayer support and counseling, the chief psychiatrist thinks the prospects for the proposed collaboration are great, citing the example of Edumfa prayer camp in the Central region which currently has an ambulance for referring patients to the Accra Psychiatric Hospitals upon consultation with doctors.
In the advocacy build up to the passage of the law, one key concern of some health experts had been the fear that in proposing a mental health service, an unnecessary parallel structure was being drawn with the Ghana Health Service. I put the question to Dr Osei as to how these experts are responding to the new legal and regulatory reality. “With the passage of the law, they have all turned into advocates. They realize they have to conform. The days for your doubts are over. In any case, I never hesitate to remind them when they express doubts etc, that it is no longer a question of what they like or don’t like. It is now a matter of law which we would all have to live by. ” Further, Dr Osei argues that apart from the national level where one could make this case for parallel structures, all efforts are underway to integrate mental health care into regular care at the operational levels.
Currently underway is training for medical assistants of psychiatry and as a positive sign of the new spirit of collaboration, discussions are already in progress with Ghana Health Service authorities to incorporate them into Regional and District hospitals. Also under consideration is a plan to establish psychiatric wings in all regional and district hospitals. Further, within the Ghana Health Service, a focal person for mental health has also been appointed within its Institutional Care Division.
How has all this been possible and who have been the strongest advocates?
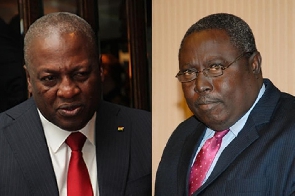
It would be recalled that following the floundering fortunes of mental health care in Ghana, the National Democratic Congress in 2008 made a manifesto promise to “To speed up the passage of a Mental Health Bill that will comprehensively change the management of Mental Health in Ghana within three months of assuming office.” After 2009, at a World Assembly meeting to tackle global health issues, there was a side meeting of “the Yale Group” with Ghana being represented by Hon Rojo Mettle Nunoo, Deputy Minister of Health, Dr Akwasi Osei, the Chief Psychiatrist, the acting Director General of the Ghana Health Service and His Excellency John Dramani Mahama, then vice president of Ghana. This meeting added further impetus to the drive for mental health reform by offering the opportunity for the burning platform to be clearly articulated , appreciated and high level political buy in achieved.
Kudos is thus due both the government for delivering on its manifesto pledge and to the many other advocacy groups under the umbrella of the Coalition of Advocates for Mental Health reform in Ghana who fought relentlessly to make this a reality.
Dr Osei is quick to acknowledge the usefulness of the pressure exerted on policy makers and politicians through a persistent media campaign and advocacy. “We never stopped saying the very things that some people hated to hear which is why today, we have a law with a difference in the sense that very few laws have taken so long to pass. One Minister of Health once told me that not one day passes by without one group or the other sending him a letter on the mental health situation.”
More specifically, Dr Akwasi Osei is grateful to all these advocates who continue to show support and are clearly in it for the long haul. Among the tall list is the Ghanaian media, civil society groups, massive international community support, mental health practitioners, Association of users and the Ghana Medical Association.
Given the real shortages in actual mental health professionals on the ground, I end my interview provoking Dr Akwasi Osei. Will anything really change in the future of mental health? As it turns out, Ghana’s chief psychiatrist had a ready-made answer for me.
“We have 14 psychiatrists now. In 5-10 years, we hope to train 80-100. We have eight Medical Assistants in Psychiatry now. We hope to train 50-80 in 5-10 years. We have three clinical psychologists in public health service now. We hope to train 50-80 in 5-10 years. We have no occupational therapists now. We hope to train 20 in 5-10 years. We have 600 psychiatric nurses now. We hope to train more than 4000 in 5-10 years. We will do this either through expanding existing facilities or establishing more or both”
Sodzi Sodzi-Tettey
www.sodzizsodzi.com
sodzi_tettey@hotmail.com
7th September 2012
Health News of Tuesday, 11 September 2012
Source: --