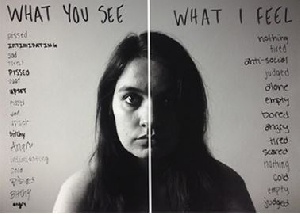
Depression is a complex mental health condition that affects millions of people worldwide, casting a shadow over their lives. It is often described as a mood disorder, but its roots run deep within the intricate circuits of the brain. Depression, often described as a silent battle, affects millions of individuals worldwide, transcending age, gender, and socio-economic boundaries.
As a doctor, my life's work is dedicated to understanding the intricate workings of the human brain. Depression, I have come to learn, is not merely a psychological ailment; it has profound neurological underpinnings.
In this article, we will delve into the neurological aspects of depression, shedding light on the brain's role in this condition and exploring cutting-edge research that may pave the way for more effective treatments.
Depression is a mental health disorder that profoundly affects mood, cognition, and behavior. Although it has been traditionally considered a psychiatric illness, modern neuroscience has unveiled the pivotal role of the brain in its development and progression. Multiple areas of the brain are involved in the complex interplay of factors contributing to depression. One of the key neurological aspects of depression is the role of neurotransmitters—chemical messengers that transmit signals between nerve cells.
In particular, serotonin, norepinephrine, and dopamine are implicated in mood regulation. Imbalances in these neurotransmitters can significantly contribute
to the development of depressive symptoms. One of the key neurotransmitters that plays a central role in depression is dopamine. In this article, we will explore the relationship between depression and dopamine, shedding light on how this neurotransmitter influences our emotional well-being and the potential treatment implications.
Dopamine is a neurotransmitter—a chemical messenger—that plays a critical role in regulating mood, motivation, and pleasure. It is often referred to as the "feel-good" neurotransmitter because of its role in creating a sense of reward and happiness. However, when the dopamine system is disrupted, it can contribute to the development and persistence of depressive symptoms.
Dopamine operates in several pathways within the brain, including the mesolimbic
and mesocortical pathways, which are closely tied to the experience of pleasure and motivation.
When these pathways are functioning optimally, they contribute to feelings of joy, satisfaction, and an overall sense of well-being. In the context of depression, one of the critical aspects of dopamine dysfunction is the brain's
reward system. People with depression often exhibit altered responses to rewarding stimuli. In essence, their brains have difficulty experiencing pleasure and motivation, which are hallmark features of depression. Anhedonia, the inability to feel pleasure in activities once enjoyed, is a prominent symptom of depression.
This phenomenon is thought to be closely linked to dopamine dysfunction. When the dopamine system is not functioning, as it should, individuals may struggle to find joy in experiences that were previously fulfilling.
While the precise mechanisms underlying dopamine imbalances in depression are still under investigation, several factors have been identified: Some research suggests that individuals with depression may have reduced dopamine release in key brain regions. Abnormalities in dopamine receptor density or sensitivity may contribute to depressive symptoms.
Chronic stress, a known risk factor for depression, can disrupt dopamine regulation in the brain. Genetic factors also play a role in the development of depression, including the regulation of dopamine-related genes.
Understanding the dopamine-depression connection has significant implications for the treatment of depression. Many antidepressant medications, such as selective serotonin and norepinephrine reuptake inhibitors (SSRIs and SNRIs), indirectly influence dopamine pathways. They work to restore the balance of neurotransmitters in the brain, including dopamine, which can help
alleviate depressive symptoms.
Additionally, therapies like cognitive-behavioral therapy (CBT) and mindfulness-based approaches have been shown to have a positive impact on the dopamine
system by addressing dysfunctional thought patterns and behaviors associated with depression.
The prefrontal cortex, the brain's executive center, is responsible for decision-making, problem-solving, and regulating emotions. In individuals with depression, there is evidence of reduced activity in this region, which can lead to difficulty in regulating negative emotions and maintaining cognitive flexibility. The hippocampus is a region vital for memory and emotional
regulation, experiences atrophy in those with depression.
This shrinkage may be linked to the reduced number of new neurons generated in the hippocampus—a process called neurogenesis. The impairment of neurogenesis has been associated with the development of depressive symptoms. The amygdala, the brain's emotional center, plays a crucial role in processing and
modulating emotions. In individuals with depression, this region tends to be hyperactive, leading to heightened emotional responses to stressors and negative stimuli.
Emerging research suggests that neuroinflammation may contribute to depressive symptoms. Chronic inflammation in the brain is associated with changes in neurotransmitter function and may play a role in the development of depression.
Genetics also plays a substantial role in depression. Studies have identified specific genes that are linked to the condition, making some individuals more susceptible to it.
The interplay between genetic predisposition and environmental factors further complicates the neurological underpinnings of depression. Understanding the neurological aspects of depression has led to the development of more targeted and effective treatment approaches. Medications like selective serotonin reuptake inhibitors (SSRIs) and norepinephrine-dopamine reuptake inhibitors (NDRIs) aim to restore the balance of neurotransmitters in the brain.
These drugs, in combination with psychotherapy, have shown considerable success in managing depressive symptoms. Furthermore, novel treatments like transcranial magnetic stimulation (TMS) and ketamine infusions are providing promising results for individuals with treatment-resistant depression.
TMS involves the use of magnetic fields to stimulate specific regions of the brain, while ketamine is believed to have rapid-acting antidepressant effects on the brain's glutamate system. Depression is a multifaceted mental health condition with complex origins. Dopamine, as a crucial neurotransmitter, plays a pivotal role in the brain's reward system and emotional regulation. Imbalances in dopamine function can contribute to the development and persistence of depressive symptoms, particularly anhedonia and reduced motivation.
Understanding the connection between depression and dopamine offers valuable insights into potential treatment strategies. Medications and therapies that address dopamine imbalances, along with lifestyle adjustments, can contribute to the restoration of emotional well-being in individuals battling the blues. Depression remains a formidable adversary, but with research continuing to unveil the complexities of this condition, there is hope for improved treatments and a brighter future for those affected by it.
Depression is a complex condition with deep-seated neurological origins. Understanding the brain's role in depression is essential for developing
more effective treatments and interventions. While there is still much to uncover, the field of neuroscience continues to make significant strides in unraveling the mysteries of depression.
The hope is that these discoveries will lead to more targeted, personalized, and ultimately successful treatments for individuals grappling with this often debilitating condition. Depression may be a formidable foe, but with advancing research and the dedication of the medical community, there is hope for a brighter future for those affected by this condition.
Health News of Thursday, 16 November 2023
Source: Simon Badu, Contributor