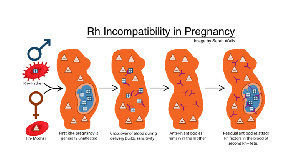
Rhesus factor incompatibility, commonly referred to as Rh incompatibility, is a condition that can occur during pregnancy when the blood types of a pregnant woman and her baby or fetus do not match.
The difference in blood type, if not properly managed, can result in a notable health risk for the unborn child.
Understanding Rh incompatibility, its possible consequences, and management, is imperative for expecting parents and soon-to-be couples, a report by the Cleveland Clinic said.
Rhesus Factor
The Rhesus (Rh) factor is an inherited protein found on the surface of red blood cells. A person who has no protein on his or her Red Blood Cells (RBC) is Rh negative.
Likewise, if you have the protein on the surface of your RBC, you are Rh-positive.
According to research, about 85% of the population is Rh-positive, while the remaining 15% are Rh-negative.
What is the cause of Rh Incompatibility?
Rhesus factor incompatibility happens when an Rh-negative woman conceives an Rh-positive fetus.
In this case, the mother’s immune system sees the baby’s Rh-positive red blood cells as foreign bodies, hence the mother's immune system produces antibodies that pass through the placenta to fight the fetal blood cells.
This further leads to the destruction of the fetus's red blood cells; which is a type of anemia called hemolytic anemia.
Mothers usually do not experience this type of complication during their first pregnancy. The reason is that it is rare for a pregnant woman's blood to mix with the fetus’s blood until delivery, which simply means there will be no formation of antibodies till after the fetus is born.
Risk factors associated with Rh incompatibility
The red blood cells of the fetus are destroyed by hemolytic anemia faster than it can replace them.
The risk or effects varies from mild to severe. They include:
a. Anemia: Destruction of red blood cells that leads to a severe shortage of these cells.
b. Jaundice: As red blood cells break down, they release bilirubin, leading to jaundice, characterized by yellowing of the skin and eyes.
c. Hydrops Fetalis: is a condition in which large amounts of fluid build up in a baby's tissues and organs, causing extensive swelling
d. Stillbirth
e. Liver failure
f. Heart failure
Diagnosis and Monitoring
Regular care includes blood tests to determine the mother's Rh status.
If a mother is found to have an Rh-negative status, the father's Rh status may also be tested.
If the father is Rh-positive, there is a possibility of Rh incompatibility, and the pregnancy will be monitored closely.
Pregnancy requires careful monitoring in instances where antibodies have already developed. There can also be an early delivery if the baby's condition is worse or an intrauterine transfusion to treat anemia before birth
Prevention and Management
Rh immunoglobulin (RhIg), commonly referred to as RhoGAM is a preventive treatment that can effectively be used to manage RH incompatibility.
RhIg is an injection given to Rh-negative mothers to prevent the formation of antibodies against Rh-positive blood cells.
Rhlg is an injection administered during 28 weeks of pregnancy and repeated within 72 hours after delivery if the baby is Rh-positive.
(Some of the details captured in this article are sourced from myclevelandclinic.org and acog.org)
RAD/AE
Click to view details


Health News of Wednesday, 21 August 2024
Source: www.ghanaweb.com
Rhesus Factor Incompatibility: Understanding what it is, the risks and management
Opinions