Concern is mounting in Africa over the growing number of well-educated and much-needed nurses who are leaving the continent for better salaries and working conditions in Britain.
The British nursing register shows the number of nurses being certified from Botswana, Ghana, Malawi, Nigeria, Kenya, South Africa, Zambia and Zimbabwe -- all former British colonies -- has soared since 1999.
As a result, more than 60 per cent of nursing positions remain unfilled in countries such as Ghana and Malawi.
"It's been catastrophic," says Dr. William Aldis, who represents the World Health Organization in Malawi. "The nurses are the ones to hold the situation together at hospitals and they are all leaving."
Sub-Saharan Africa's low-income countries need to more than double their work forces, adding at least 620,000 nurses to be able to tackle the severe health emergencies, according to estimates by the Joint Learning Initiative. The network is coordinated by Harvard University and consists of more than 100 scholars and analysts studying human resources for health.
The nursing shortage is intensifying as foreign aid is beginning to pour into Africa to provide life-saving drugs to millions of people afflicted with AIDS and tuberculosis.
The money includes the first installment on a total of $15 billion promised by U.S. President George W. Bush and $2 billion from the Global Fund to Fight AIDS, Tuberculosis and Malaria.
By 2006, Britain is aiming to increase its aid to Africa from ?711 million ($1.29 billion) to ?1 billion ($1.82 billion).
Ironically, African countries need more nurses in order to utilize the new funding.
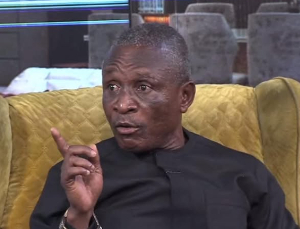
"The money will not be of any use if there are no nurses to administer the drugs," says Dr. Dela Dovlo, former director of human resources at Ghana's Ministry of Health.
New rules for recruitment In 2001, Britain recognized the increasing problems in Africa and adopted codes to limit the government's active recruitment of health professionals from developing countries.
But the codes do not apply to private recruitment agencies or private employers. Nor does it prohibit the National Health Service from hiring African nurses who apply on their own. Since the new codes came into effect, more than 7,000 African nurses have registered to work in Britain.
"The effects of the outflow of health professionals has led to the phenomenon of a brain drain," says Dr. Barbara Stillwell, a scientist with the WHO's department of human resources for help in Geneva. "The poor African countries are subsidizing the richer countries with nurses."
Stillwell would like to see more restrictions put in place: "There should be agreements between countries. Nurses should be given the opportunity to migrate, but only for a specific length of time. Two-year contracts could be used to make sure they come back."
However, Stillwell says she recognizes that it would be against human rights to stop people from moving.
According to the Department of Health in Britain, there is little more the UK government can do to prevent the continued migration of African nurses.
"They come because of huge push factors and we can't stop this. Also, it is very difficult to stop private recruiters from recruiting there, but we will soon announce a new clamp down strategy," a government official said.
Chance to better their lives While acknowledging the severe shortage, NHS nurse Rose Haldane says it is only fair that hard-working African women be given a chance to better their lives.
Haldane, who leads a newly developed overseas nurse adaptation course for the Guy and St. Thomas NHS foundation trust in London, says: "African nurses go through a tough recruitment process to get here.... They have made the choice to change their life and we are pleased to give them this chance."
One of Haldane's students worked as a nurse in Nigeria for three years before she decided to come to London.
"They have less equipment at home and nursing is very hard there. Where I was there were 32 beds on a ward with only three qualified nurses. Here there are 27 beds on a ward with six nurses. London is much better."
Another student, a nurse from Sierra Leone, added: "The equipment is better in the UK. In Sierra Leone, we had to improvise due to the lack of equipment. Here in England we have everything we need to treat the ill."
But the departure of young to Britain, has long been a sore subject with Britain's former African colonies.
"Its like a vicious circle," says the WHO's Dr. Aldis. "As more nurses leave the hospitals, the work conditions worsen for the remaining nurses and as a result they are more tempted to leave as well."
Dr. Dovlo, the former Ghana health official, says Africa's future looks bleak if nurse migration continues. "The shortage is likely to dismember the whole health system in Africa," he says.
General News of Wednesday, 4 August 2004
Source: CNN